Many buyers of surgical gowns struggle to understand which parts of the gown are truly safe for sterile use. This confusion can cause mistakes in the operating room and even increase the risk of infection. To avoid costly errors, it’s important to know the sterile areas of a surgical gown and how they are designed to protect both patients and staff. This guide explains the critical sterile zones step by step.
Sterile Areas of Surgical Gowns: My Guide to Infection Control
To stop surgical infections, I think it’s vital to know which parts of a surgical gown are sterile and why. We must guard the sterile field carefully. Any mistake increases the risk of infection. Here is what I believe the latest data and guidelines point out:
Sterile Areas of Surgical Gowns
1.Front Panel (Chest to Mid-Thigh/Table Level)
I consider the main sterile zone to be the front of the surgical gown. This area runs from your chest down to your mid-thigh or table level.
Based on my review of the data, studies on 50 spinal surgery gowns showed that this area was the cleanest. Yet, some contamination (6–48%) still occurred.
I recommend following AORN guidelines. If you touch your shoulder, back, or below your mid-thigh, you have broken sterile protocol.
2.Sleeves (Cuff to 2 Inches Above Elbow)
I believe the sleeves are sterile from the cuffs up to two inches above the elbow. This does not include the shoulders.
I suggest you avoid contact with the elbow crease; data shows a contamination risk there.
At any point, if a sleeve touches a non-sterile surface, my experience shows the gown and gloves must be replaced.

Non-Sterile Areas of Surgical Gowns
1.Back, Shoulders, and Below Tabletop/Mid-Thigh
In my opinion, the back of the disposable surgical gown, the shoulders, and anything below table level are not sterile.
AORN and CDC guidelines require you to avoid touching these areas.
I advise you not to turn your back on the sterile field. The back can get contaminated easily.
2.Clothing Protruding from Gown
If your personal clothes stick out from the neck or sleeves, this is a contamination risk. I feel this should not be allowed in the sterile field.
My Observations & Data Points
Based on my experience, if you turn your back on the sterile field, the gown needs an immediate change. This also applies if a sleeve touches a non-sterile surface.
I’ve seen data showing higher contamination rates at the elbow. This also happens at 24 inches or less and 48 inches or more from the ground.
I’ve found that sterile surgical gown areas can get contaminated during long surgeries or with a lot of movement. The contamination rates are higher after the procedure is finished.
Sterile Gown Area Quick Reference Table
| Gown Area | Sterility | My Comments/Key Data |
|---|---|---|
| Front panel (chest to mid-thigh/table) | Sterile |
Lowest contamination (6–48%), based on my review of the data. |
| Sleeves (cuff to 2 inches above the elbow) | Sterile |
Elbow creases are at a higher risk; I see this as a firm boundary. |
| Back, shoulders, below the tabletop | Non-sterile |
Higher contamination, I suggest you avoid this area in surgery. |
From my perspective, following these sterile surgical gown boundaries is key to keeping the operating room safe. It also helps lower the risk of infection, a view supported by studies from AORN and CDC.
How do We Sterilize Surgical Gowns?
Main Ways We Sterilize Surgical Gowns
From my experience, to keep surgical gowns safe, we must use proven sterilization methods. These methods ensure the sterile parts of the gown meet medical safety rules. I’ll walk you through the main techniques we use:
Steam Autoclaving: I find this is the most common way to sterilize reusable gowns. We use an autoclave. This machine uses high-pressure steam at 121–134°C for 15–30 minutes at 15–30 psi. For a quicker option, we can use 134°C for just 3–5 minutes. I recommend this for any gown that can handle high heat and steam.
Ethylene Oxide (EtO) Gas: What about disposable surgical gowns or materials that can’t take the heat? For those, I suggest using EtO gas. We process them at a lower temperature of 37–63°C for 2–16 hours. After that, they need to air out for 8–24 hours to clear any gas. EtO provides a deep clean, but it does take more time.
Gamma Irradiation: For mass-produced disposable gowns, we often use gamma irradiation. We apply a dose of 15–25 kGy. The great thing about this method is that it goes right through sealed packages. This lets us sterilize huge batches at once without heat or moisture damage.

Quality Control and Making Sure Gowns Are Sterile
In our quality control, we aim for a Sterility Assurance Level (SAL) of 10^-6 for all sterile areas. I like to think of this as our guarantee. It means there’s less than a one-in-a-million chance of finding a single living microbe on a gown. To make sure we hit this target, I recommend these checks:
Biological Indicators: We place spore strips or vials inside the gowns. After the cycle, we test them. If nothing grows, we know all microbes were destroyed.
Chemical Indicators: I suggest using special strips or labels on or in the packages. They change color when the right sterilization conditions are met. This gives us a quick visual check.
Physical Monitoring: Our equipment tracks everything. It records the temperature, pressure, and time for each cycle. This gives us a complete data log for every single batch.
My Quality Checks After Sterilization
After the main process, I always perform extra quality checks. These steps make sure the critical sterile areas of the surgical gown remain sterile:
- We look over the packaging for any holes or tears.
- We swab random gowns and test the swabs for any living microbes.
- I double-check the data from every cycle. I confirm the temperature, time, and concentration were correct.
- We document everything. This includes the lot number, production date, sterilization method, and expiration date for disposables.
We do regular audits and test each lot before it goes out. This is how we follow the rules set by groups like the FDA, AAMI, and ISO.
How do We Handle Disposable vs. Reusable Gowns?
- Disposable Gowns: These arrive sterile in their sealed packages from the factory. You use them once after opening and then dispose of them. They should never be sterilized again.
- Reusable Gowns: After each use, we have a clear process. We clean the gown, check it for any damage, and then sterilize it all over again. We also repeat all the quality control checks.
In my opinion, following these steps is crucial. They protect the sterile parts of the gown. This creates the barrier we need to reduce the chance of infections during surgery.
Best Practices for Maintaining Sterility in Surgical Gown Zones
From my experience, effective infection control depends on how you handle, store, and use disposable sterile surgical gowns. I suggest following these steps to keep gowns sterile during surgery:
Proper Donning and Doffing Technique
- I always start with a complete surgical hand scrub.
- Use a careful, sterile method to open the surgical gown pack.
- Touch just the inside of the gown when picking it up. Never touch the sterile outer surface.
- Slide your arms into the sleeves. Be sure your hands do not go past the cuffs.
- A sterile assistant should fasten the surgical gown’s back. In my view, the back is never sterile.
- I recommend closed gloving. Keep your hands inside the gown sleeves until the gloves are on correctly.
- To take the surgical gown off, remove your gloves first. Use the glove-to-glove, then skin-to-skin technique.
- Untie the gown and pull it off, turning it inside out. Make sure you touch just the inside surface.
- Throw away the gown and gloves in the right waste bins right after you take them off.
Gown Storage and Transport Guidelines
I suggest storing sterilized surgical gowns in closed spaces. The temperature should be 15–30°C with humidity under 60%.
To prevent contamination, I always transport gowns in sealed, sterile packages.
Never put the package on any surface that is not sterile or is wet.
You should use the FIFO (first in, first out) method to rotate your stock. This means using older gowns first to maintain sterility.
Staff Training and Protocol Enforcement
I believe it’s crucial to hold hands-on training and skill tests for gowning at least once a year.
I recommend using drills that simulate contamination. This helps staff practice correct handling and find common errors. For example, they might touch the outer surface or let sleeves touch unsafe areas.
Make sure all team members know the sterile zones. These are the front of the body from mid-chest to table level. It also includes the sleeves from 2 inches above the elbow to the cuff.
Using visual aids is a great idea. I also suggest regular audits to check that everyone follows correct procedures.
Common Errors and How to Prevent Them
Never touch the outside of the surgical gown with your bare hands while putting it on. From my experience, this is a major source of contamination.
Keep the surgical gown’s sleeves and skirt away from tables, equipment, and the floor.
Do not refold a gown. If you do, the inside and outside surfaces might touch before you put it on.
Stay close to the sterile area. If you step away, you might touch non-sterile things with your back or lower body.
If you think your gown or gloves are contaminated, you must change them right away.
Correction and Prevention Methods
I recommend assigning a nurse or observer to watch the gowning process. They can correct mistakes as they happen.
Mark high-risk areas beforehand. It is smart to have a “stop and re-gown” rule if any contamination is spotted.
You should inspect all stored surgical gowns before use. Check the package for damage and check the expiration date. Throw away any that are damaged or expired.
The Role of Checklists
In my opinion, every staff member should use a detailed checklist before, during, and after surgery:
- Check the surgical gown’s package and sterility.
- Make sure surgical gowns are stored right and FIFO is used.
- Follow every step for putting on and taking off the gown.
- Write down any mistakes and the steps taken to fix them.
Data shows that using checklists helps. It lowers growth rates after surgery. Audits across multiple centers found a reduction of up to 37% in six months.
Real-World Data and Key Figures
Studies find contamination rates can be high. They reach up to 48% at the sleeve elbow, and if the gown is at the wrong height. The rate is as low as 6% at the chest, which shows why knowing sterile boundaries is key.
For surgeries like lumbar spine cases, a surprising fact is that over half of contaminated gowns were exposed during the gowning process itself, not just during the surgery.
When you put checklists and training into practice, I have seen a big drop in reported mistakes. This greatly improves overall sterility.
FAQs for Sterile Surgical Gown
Are surgical gown sleeves sterile?
Yes, sleeves are sterile from the cuff to 2 inches above the elbow. The elbow crease and shoulders are not sterile. Always avoid touching non-sterile surfaces.
Can disposable gowns be re-sterilized?
No. Disposable surgical sterile gowns come pre-sterilized and should be used only once. Re-sterilizing can damage the material and increase infection risk.
What is the cleanest part of a surgical gown?
The front panel, from the chest to mid-thigh or table level, is the cleanest. This area has the lowest contamination rates (around 6–48%).
How should sterile gowns be stored?
Store gowns in a clean, dry area at 15–30°C with humidity below 60%. Keep them in sealed packages and use older stock first (FIFO method) to maintain sterility.
Can I touch the outside of the gown while donning?
No. Only touch the inside of the gown when putting it on. The outer surface is sterile and any contact can cause contamination.
How do I know if a gown is still sterile?
Check the package for damage or tears, and look for expiration dates. Many gowns have chemical indicators that change color when sterilized.
Are reusable gowns safe?
Yes, if properly cleaned, inspected, and sterilized after each use. Always follow the recommended sterilization method and quality checks.
What should I do if I suspect contamination?
Immediately change your gown and gloves. Even small contact with non-sterile surfaces can increase infection risk.
How to Get High-Quality Sterile Surgical Gowns?
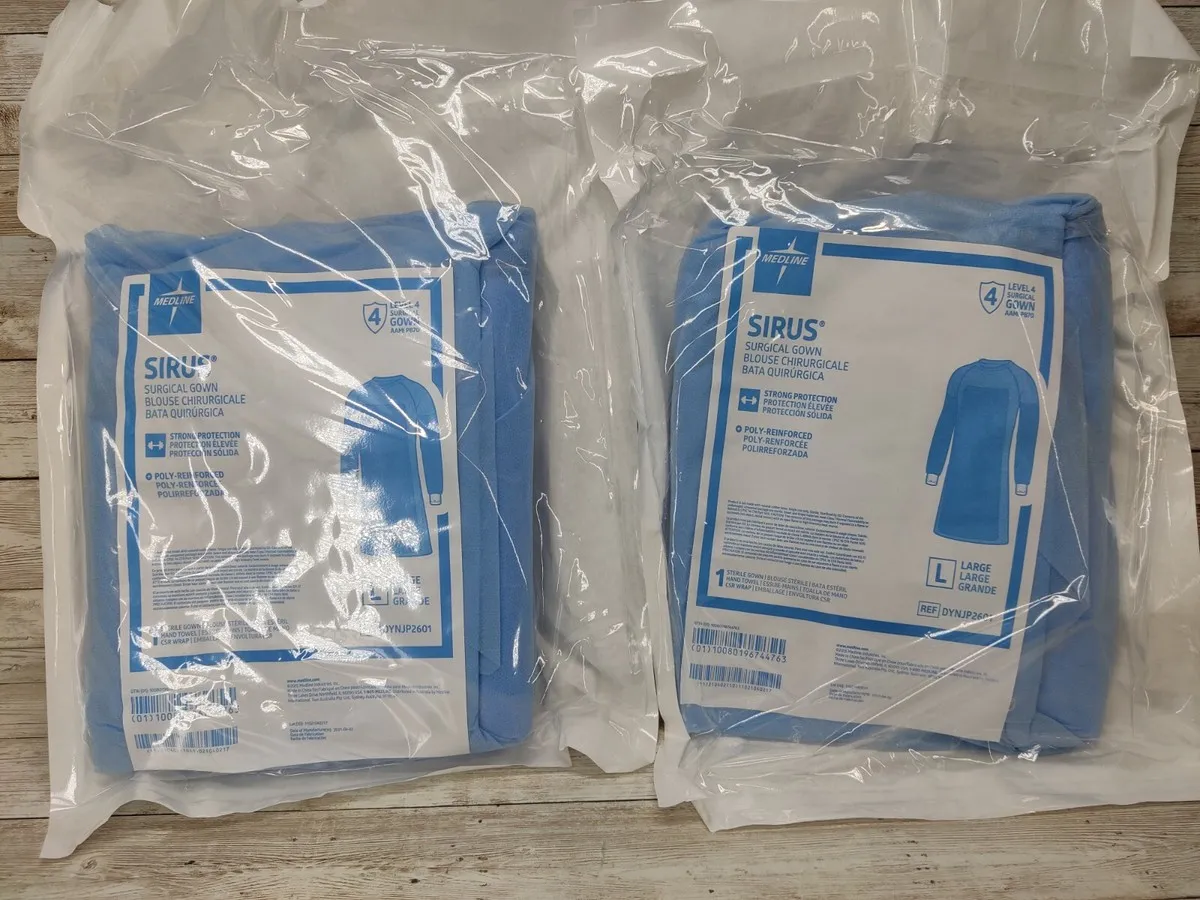
Morntirp provides sterile surgical gowns that meet AORN, AAMI, and ISO standards. We offer both disposable surgical gowns suitable for hospitals, clinics, and surgical centers.
All disposable surgical gowns are carefully sterilized, inspected, and packaged to ensure the sterile areas remain safe. Buyers can request detailed product specifications, batch testing data, or packaging options to meet their operational needs.
For larger orders, Morntirp supports OEM and ODM services, with reliable global shipping and first-in, first-out (FIFO) stock rotation guidance to maintain sterility during transport.
By choosing a trusted sterile surgical gown manufacturer, hospitals and distributors can ensure consistent product quality, reduced infection risk, and compliance with international standards.